Peroneal Tendon Disorders
What are the peroneal tendons?
The peroneal tendons (arising from the peroneus longus peroneus brevis muscles) are two tendons that run behind the outer bone of the ankle (lateral malleolus or fibula). The tendons lie within a sheath which restrains them as they pass behind the the ankle joint they run down the outer border of the heel and attach to bones in the foot. The peroneal tendons are responsible for pulling the foot outwards and have a very important role in stabilising the ankle joint.
How do peroneal tendons cause problems?
Many patients remember a traumatic episode - most commonly an ankle sprain. Some patients develop pain without trauma. Certain conditions also predispose to peroneal tendon injuries such as cavo-varus (high-arch) foot, inflammatory arthritis, diabetes and steroid injections.
The tendons may become inflamed (tendinosis/tenosynovitis) or develop splits within them. Repetitive trauma may eventually cause the tendon to rupture.
The injured tendon produces pain and swelling along the outside of the ankle/foot, occasionally they may become weak which results in a tendency for the ankle to give-way on uneven ground.
Occasionally a sprain may cause the peroneal tendons to dislocate, where the sheath surrounding the tendons is damaged so that the tendons dislocate round the side of the fibula during ankle movements. This is characterised by a painful 'clicking" feeling along the outside of the ankle as the tendons dislocate from their normal positions and sometimes a feeling of ankle weakness.
How can they be diagnosed ?
Most peroneal tendon injuries may be diagnosed by careful examination. An ultrasound or MRI scan are useful to assess the tendons further. An X-ray is useful to assess the ankle region for arthritis or traumatic changes that may contribute to the pain..
What is the treatment
The aim of treatment is to relieve pain and prevent further injury to the tendons.
In most cases non-surgical treatment is attempted first - this includes modifying footwear , insoles, and anti-inflammatory medication to reduce pain and inflammation. Changing the type or intensity of your activity may also help . Acute injuries and inflammation of the tendon sheath frequently respond to non-operative therapy.
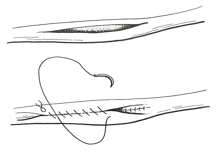
Long-standing tendon tears and dislocating tendons, however, often require surgery. This is a an operation that involves repair of the tendon tear with a fine suture. A severely damaged tendon may need to be excised and re-attached to one of the other tendons so that its function may be preserved.
Figure {C}1{C}
{C}{C}
If the tendons are dislocating then the sheath must be reconstructed at the same time the shallow groove that the tendons run along as they pass behind the ankle may need to be deepened. After surgery the ankle is normally placed in a plaster cast for 4 weeks and a supportive ankle brace for another 8 weeks. Physiotherapy plays a very important role after the plaster is removed..
Surgery for peroneal tendon disorders has 80-90% good or excellent results, although success obviously depends upon the severity of the tears. Patients are usually able to return to previous recreational and sporting activities.
Are there any risks of surgery?
As with all foot and ankle surgery, peroneal surgery carries a small risk of complications. As well as the standard risks of infection, wound breakdown, nerve injury and bleeding peroneal surgery carries the specific risk of dislocation of the tendons, this is why the post operative plaster and subsequent physiotherapy are so important.
Be sociable..share!